About 4 of 5 large US employers offer wellness programs as part of their employees’ health benefits. The goals are admirable, viz., support employees in changing health behaviors that reduce their risk for certain chronic conditions and enable those with existing conditions to manage them more effectively. Such programs typically include health assessments and biometric screening to quantify risk factors; education and coaching for lifestyle behavior modification (e.g., tobacco cessation, physical activity promotion, stress reduction, and weight management); and less often chronic disease management. These programs are based upon the assumption of producing health and economic benefits which might lower medical care spending to lower the cost of employer-sponsored insurance premiums. Further, healthier employees should be less likely to miss work due to illness and be more productive while at work. Stronger employee engagement, reduced turnover, and improved profitability are other perceived goals.
The total cost of a wellness program is between $150 and $1200 per employee per year depending upon options an employer wants to include. Many wellness vendors offer a comprehensive wellness program that uses a proprietary wellness platform which costs between $3 and $7.5 per employee per month ($36 -$90/ year). These usually include a mobile app and website that provides a health risk appraisal, incentive management, online resources, culture change, wellness campaigns and team challenges, and integration of fitness devices.
But do all these benefits lead up to the hype? A rigorously conducted wellness program offered to a large workforce over an 18-month period, included 8 sequentially delivered modules instructed by dietitians, each of 4 to 7 weeks in duration, covered topics such as engaging with the health care delivery system, nutrition, exercise, stress management, sleep, and weight management. Employees who completed a given module received a financial incentive (e.g., $25 gift card) Approximately 35% of employees completed at least 1 module, and among those who did, the mean number of completed modules was 3.7 of the 8.
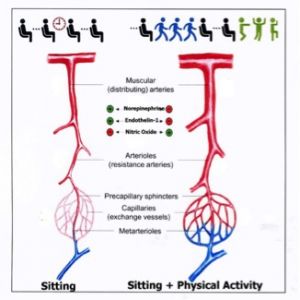
No statistically significant differences of wellness measures were detected between the employees in the control and wellness treated group at the end of the 18 months. Similarly, there were no significant differences in medical care spending, productivity, performance or utilization (Song et al: Effect of a workplace wellness program on employee health and economic outcomes, JAMA 321:1491-1501, 2019). These disappointing results might have been related to the brevity of the trial or to dilution of participant interest in the wellness activities owing to choices of too many modules [Keep it Simple Stupid!]. Perhaps corporate wellness programs should focus on cost-effective means to mitigate a limited number of lifestyle diseases and conditions that can be accomplished mainly in the home rather than the workplace. One such home wellness technology is the Gentle Jogger® as addressed in Blog #5: What do Television Viewing, Hypertension, Fibromyalgia and Opioid Addiction have in Common?